What’s Wrong with this Data?
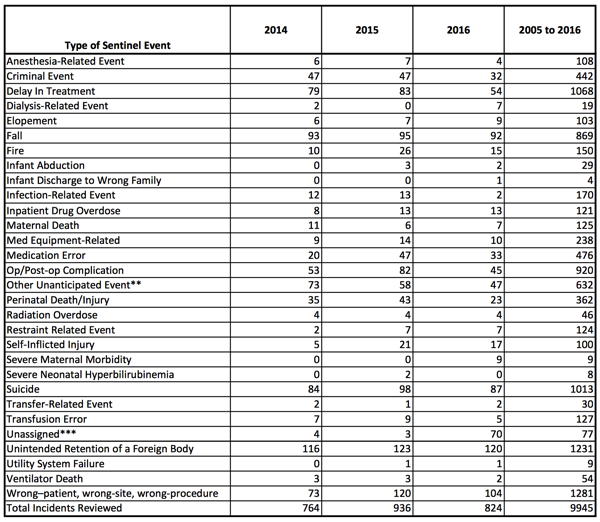
The above are sentinel event types from 2014 – 2016, as reported to the Joint Commission (taken from a 1/13/2017 report).
Reviewing this data, one might ask …
What can we learn?
I’m not trying to be critical of the Joint Commission’s efforts to collect and report sentinel event data. In fact, it is refreshing to see that some hospitals are willing to admit that there is room for improvement. Plus, the Joint Commission is pushing for greater reporting and improved root cause analysis. But here are some questions to consider.
- Does a tic up or down in a particular category mean something?
- Why are suicides so high and infections so low?
- Why is there no category for misdiagnosis while being treated?
Perhaps the biggest question one might ask is why are there only 824 sentinel events in the database when estimates put the number of sentinel events in the USA at over 100,000 per year.
Of course, not all hospitals are part of the Joint Commission review process but a large fraction are.
If we are conservative and estimate that there should be 50,000 sentinel events reported to the Joint Commission each year, we can conclude that only 1.6% of the sentinel events are being reported.
That makes me ask some serious questions.
1. Are the other events being hidden? Ignored? Or investigated and not reported?
Perhaps one of the reasons that the healthcare industry is not improving performance at a faster rate is that they are only learning from a tiny fraction of their operating experience. After all, if you only learned from 1.6% of your experience, how long would it take to improve your performance?
2. If a category like “Unintended Retention of a Foreign Body” stays at over 100 incidents per year, why aren’t we learning to prevent these events? Are the root cause analyses inadequate? Are the corrective actions inadequate or not being implemented? Or is there a failure to share best practices to prevent these incidents across the healthcare industry (each facility must learn by one or more of their own errors). If we don’t have 98% of the data, how can we measure if we are getting better or worse? Since our 50,000 number is a gross approximation, is it possible to learn anything at all from this data?
To me, it seems like the FIRST challenge when improving performance is to develop a good measurement system. Each hospital should have HUNDREDS or at least DOZENS of sentinel events to learn from each year. Thus, the Joint Commission should have TENS or HUNDREDS of THOUSANDS of sentinel events in their database.
If the investigation, root cause analysis, and corrective actions were effective and being shared, there should be great progress in eliminating whole classes of sentinel events and this should be apparent in the Joint Commission data.
This improved performance would be extremely important to the patients that avoided harm and we should see an overall decrease in the cost of medical care as mistakes are reduced.
This isn’t happening.
What can you do to get things started?
1. Push for full reporting of sentinel events AND near-misses at your hospital.
2. Implement advanced root cause analysis to find the real root causes of sentinel events and to develop effective fixes that STOP repeat incidents.
3. Share what your hospital learns about preventing sentinel events across the industry so that others will have the opportunity to improve.
That’s a start. After twelve years of reporting, shouldn’t every hospital get started?
If you are at a healthcare facility that is
- reporting ALL sentinel events,
- investigating most of your near-misses,
- doing good root cause analysis,
- implementing effective corrective actions that
- stop repeat sentinel events,
I’d like to hear from you. We are holding a Summit in 2018 and I would like to document your success story.
If you would like to be at a hospital with a success story, but you need to improve your reporting, root cause analysis and corrective actions, contact us for assistance. We would be glad to help.